Thinking about the other left lower quadrant
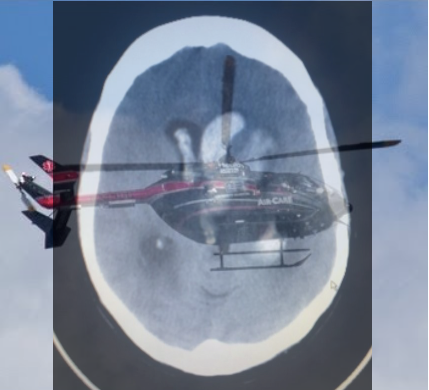
The patient is a 74 year-old African-American female with a history of hypertension, coronary artery disease status post drug-eluting stent ×1, former cigarette smoker, and iron deficiency anemia presenting with left-sided vision loss. Patient states that approximately two days ago she woke up with painless peripheral vision loss of her left eye only. She describes it as darkness in the lateral portion of her left eye. She reports that her vision returned to baseline throughout that day; only to return when she awoke the next morning. Since that time she endorses persistent vision loss in the left periphery. She denies blurry vision, eye pain, headaches, recent trauma, flashes, and floaters. Furthermore, she also denies dizziness, numbness weakness, dysarthria, dysphagia, fever, chills nausea, vomiting, chest pain, shortness of breath, and palpitations. She reports adherence to her antihypertensive and anti-platelet medications...
Read More