Grand Rounds Recap 1.10.24
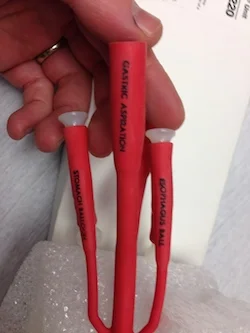
/We started off the day strong with a R4 Case Follow Up lecture presented by Dr. Yates who led an excellent discussion on psychosis, including maintaining a broad differential for secondary psychosis and appropriate management. We then transitioned to an R1 Clinical Knowledge lecture where Dr. Segev guided us through interstitial lung disease and fibrosis ranging from epidemiology to diagnosis and treatment. This then followed by a hand-on high acuity low opportunity procedure review including esophageal balloon tamponade, transvenous pacemaker placement, and chest wall escharotomy. The hands-on sessions continued into the afternoon where our CCHMC colleagues led a simulation on neonatal shock. Overall, a great day at UCEM Grand Rounds!
Read More