Induction Reduction?
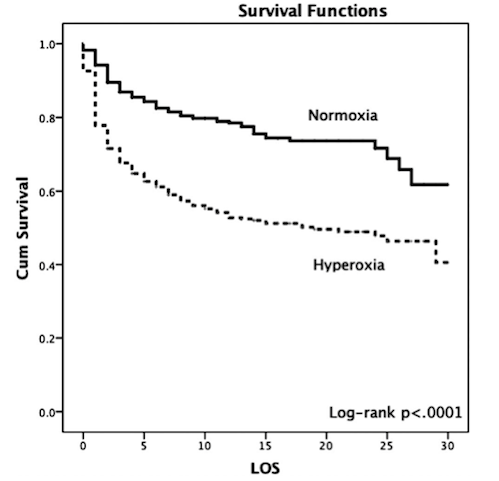
/Rapid sequence intubation (RSI) is frequently performed under emergent conditions in acutely ill patients. RSI is a technique for managing the emergency airway that induces immediate unresponsiveness (induction agent) and muscular relaxation (neuromuscular blocking agent). In properly selected patients, it is a quick, safe, and effective approach that results in optimal intubating conditions. However, one of the feared complications of RSI is post-intubation hypotension leading to cardiovascular collapse. Although there are multiple possible reasons for hypotension post-intubation, the choice and dosing of induction agents has been implicated.
Read More