A Pain in My Heart - Curated Comments and Expert Commentary
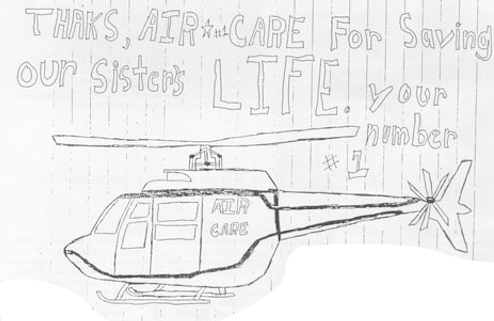
/Thanks to everybody who chimed in on our last "Flight"! We had a great discussion on the management of the STEMI transfer patient. These aren't just "milk runs" as pointed out by Dr. Hinckley. The highlights of the discussion are below with additional commentary on the case by Dr. Bill Hinckley and Air Care Resident Assistant Medical Director Dr. Matt Chinn. Out final flight will be lifting off June 1 and it's a doozy - looking forward to the discussion!
Read More