Back to Basics: Pelvic XRays
/Overview
Plain radiographs are a widely available modality that confer benefits of cost effectiveness and promptness, proving them very useful as an initial diagnostic choice when approaching several musculoskeletal concerns, particularly pelvic and hip pathologies. Pelvic and hip X-rays are almost always obtained, and with good reason, in patients presenting after significant blunt trauma to rule out bony abnormalities and underlying structural injuries in patients that are unstable or altered, have an abnormal pelvic exam, or have significant distracting injuries. While it is vital to have a high suspicion for pelvic injuries in high mechanism traumas, continue to have high concern in low energy traumas as well, especially in patients prone to pelvic injury due to underlying pathophysiology, such as the elderly or bone composition deficiencies, as they can lead to high morbidity if not diagnosed early in the course of illness.
Pelvic and hip X-rays are most frequently obtained when there is concern for fracture, joint dislocation and effusion, and several pediatric pathologies involving the pelvic girdle which are outlined below.
Before delving into the radiographic approach to pelvic and hip X-rays, let us first review some anatomy. Please review Dr. Goel’s excellent post on Pelvic X-rays that provides an excellent review on anatomy and overview on basic radiographic approach.
Pelvic and hip anterior-posterior (AP) and lateral images are most commonly obtained when assessing for pelvic bony abnormalities as many physicians have greater familiarity with interpreting these particular views. However, there are other radiographic views that can provide a more holistic view of the patient’s anatomy, allowing physicians to better visualize occult fractures that are uniquely displaced and that may not appear on the AP or lateral views. Please note that the more views that are obtained of a bone or joint, the higher the sensivity and specificity of plain radiographic imaging becomes in detecting bony abnormalities.
Hip Views
Pelvis Views
+ A/P Hip
Patient positioning
- Supine, with lower extremity of question internally rotated 15 degrees, beam shooting towards femoral head
- Allows for visualization of articulation of femur and acetabulum
Used for:
- acetabular fractures, proximal femur fractures
helps detect findings associated with Developmental Dysplasia of Hip, Legg-Calvé-Perthes, Slipped Capital Femoral Epiphysis
+ A/P Pelvis
Patient positioning
- Standing or supine, with bilateral lower extremities internally rotated 15-25° at the hip to accommodate for femoral anteversion, allowing for better visualization of the femoral neck Advantage
- Allows for evaluation of symmetry bilaterally. Also allows for evaluation of integrity of pelvic ring and shape of acetabulum Uses
- Fractures of
- anterior ring
- iliac wing
- transverse process
best depicts "open book" fractures, also known as AP compression fractures
+ Horizontal/Surgical Hip
Patient positioning:
Supine, with opposite hip flexed and abducted; place the cassette against the lateral aspect of the affected hip and aim at groin with 20 degree cephalic tilt
Allows for visualization of femoral neck
- Used for Femoral neck fractures
+ Inlet
Patient positioning Supine, with bilateral lower extremities internally rotated 15-25° at the hip, with beam shooting perpendicular to the pelvic rim at an angle of 45 degrees from cephalad to caudad. Advantage Allows for close evaluation of pelvic brim (pubic symphysis, pubic rami)
Use - imaging of the hemipelvis:
- AP translation
- Internal/external rotation Fractures:
- Pubic symphysis
- Anterior/posterior displacement of pubic rami fractures
- +/- SI joint space, sacral ala fractures
+ Frog Leg Hip
Patient positioning
- Supine, with bilateral lower extremities fully externally rotated and knees flexed
- Allows for better visualization of proximal femur, especially femoral head
- Used for Legg-Calvé-Perthes, Slipped Capital Femoral Epiphysis
Do not obtain this film if there is suspicion for hip fracture or dislocation. It may displace the fracture and worsen outcomes
+ Outlet
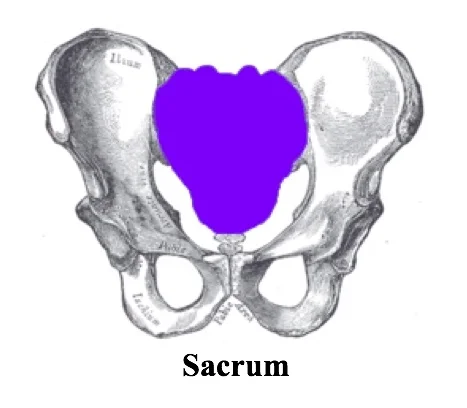
Patient positioning Supine, with bilateral lower extremities internally rotated 15-25° at the hip, with beam shooting at an angle of 45 degrees from caudad to cephalad. Advantage Allows for assessment of sacrum (SI joint, sacral foramina) Uses Hemipelvis:
- Vertical translation
- Flexion/extension Fractures of:
- sacrum and sacral foramina
+ Judet/Oblique
Patient positioning
- Supine, with beam shooting from the lateral aspect of affected hip at 40 degrees of angulation from front Advantage
- Good choice in high-energy trauma patients that are already in external rotation. Also allows for close evaluation of all surfaces of the acetabulum, as well as allow for better visualization of femoral neck Uses Acetabular fractures
Interpreting the Radiographic Pelvis
There is no one correct way in approaching a plain radiographic imaging of the pelvis or hip; however, ensure that you find an approach that allows you to evaluate each and every image in a methodical manner so as not to miss any lesions! Since I am a foodie at heart, I have chosen the mnemonic PB & JS to highlight my love of all things peanut butter and jelly.
PB & JS
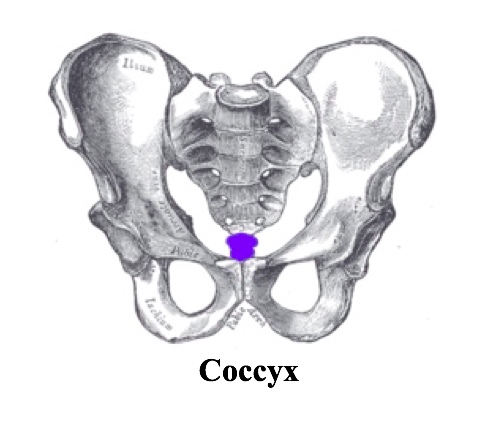
Penetration/Positioning/Patient
- Pubic symphysis and coccyx in straight line in middle of screen with 1-3cm between superior pubic symphysis and tip of coccyx
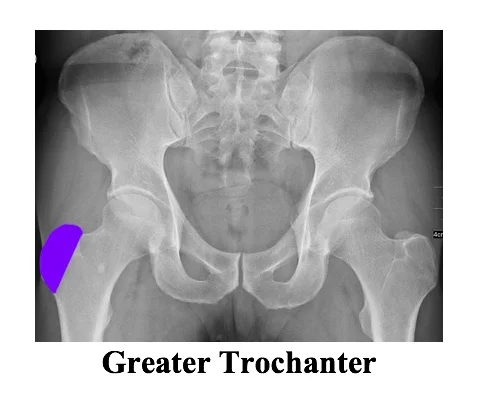
- Greater and lesser trochanters should be clearly distinguishable
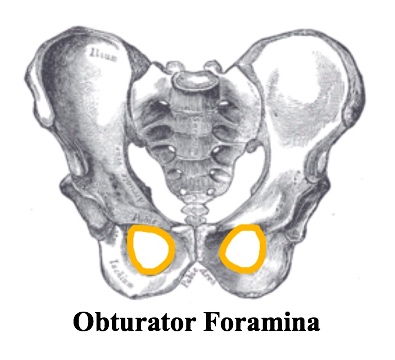
- Obturator rings symmetric
Bones
1. CORTICAL OUTLINE and BONY TEXTURE: evaluate for the integrity of the cortex throughout, as well as bony landmarks
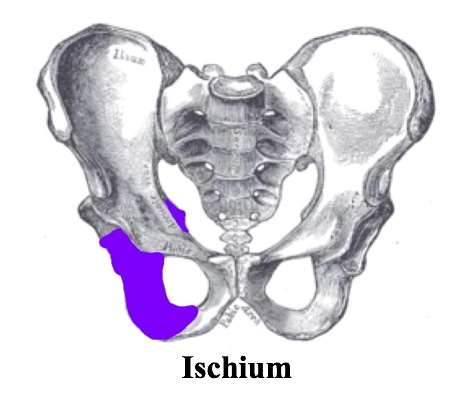
a. Pelvis
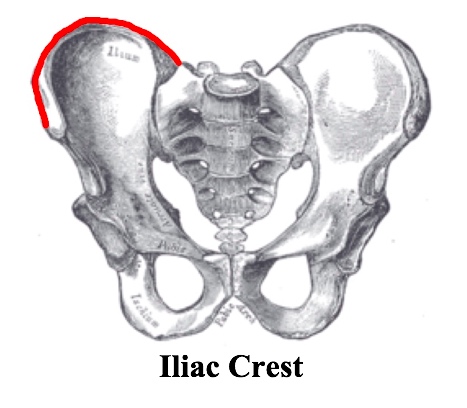
- Ilium: iliac crest, anterior superior iliac spine, anterior inferior iliac spine
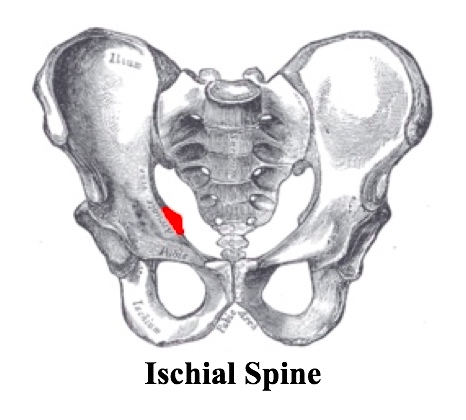
- Ischium: ischial tuberosity, ischial spine
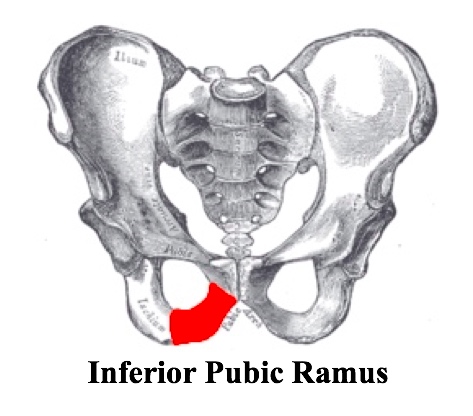
- Pubis: superior pubic ramus, inferior pubic ramus
b. Hip
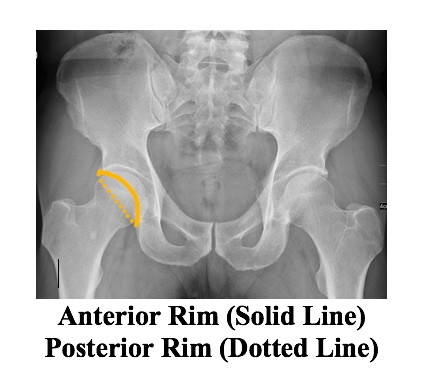
- Acetabulum: acetabular floor, anterior rim, posterior rim
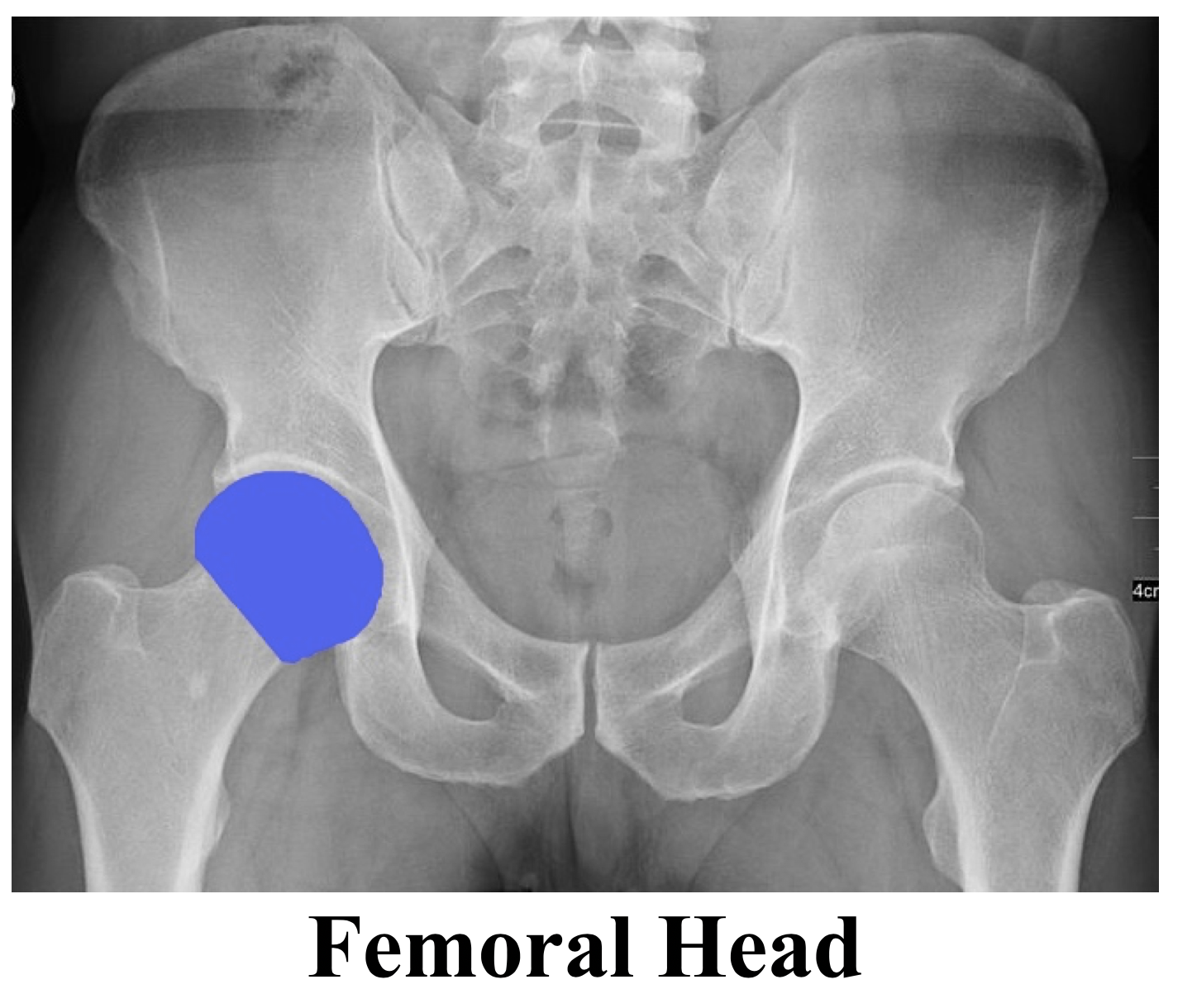
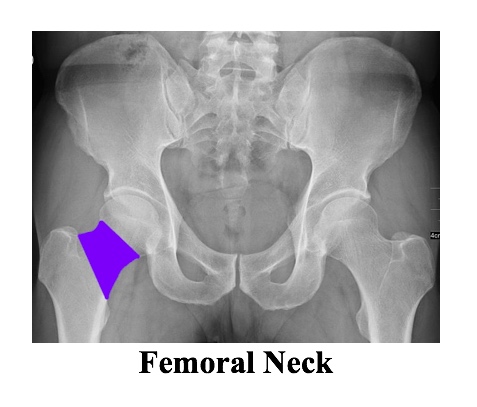
- Femur: femoral head, femoral neck, greater trochanter, lesser trochanter
2. RINGS:
- Pelvic ring
- Obturator ring, bilaterally
- Sacral foramina
3. LINES:
a. Pelvis
- Iliopectineal (Iliopubic) line
- Ilioischial line
b. Hip
- Line of Klein (line along superior femoral neck that will intersect epiphysis)
- If abnormal, may indicate slipped capital femoral epiphysis (SCFE) as under Pediatric Quick Hits
- Shenton’s arc/line (undersurface of superior pubic ramus to medial aspect of femoral neck)
- If disrupted, can indicate fracture of femoral neck
- May also indicate developmental dysplasia of hip as under Pediatric Quick Hits
- Hilgenreiner line (horizontal line connecting triradiate cartilages)
- If abnormal, may indicate developmental dysplasia of hip as under Pediatric Quick Hits
- Also used in calculating acetabular angle, as depicted in graphic below:
- Perkin’s line (vertical through lateral edge of acetabulum)
- If abnormal, may indicate developmental dysplasia of hip as under Pediatric Quick Hits
- Principal compressive trabeculae
- Principal tensile trabeculae
- If either category of trabeculae is disrupted, may indicate subcapital femoral fracture
- If either category of trabeculae is disrupted, may indicate subcapital femoral fracture
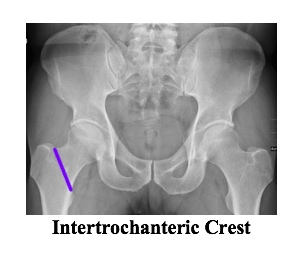
- Intertrochanteric crest: delineates between intracapsular region proximal to line or extracapsular region distal to line
- Why does it matter: Intracapsular fractures are at higher risk of avascular necrosis due to common disruption of blood supply to femoral neck with fractures in this region
- Teardrop sign (radiographic projection of bony ridge running along the floor of the acetabular fossa)
- Occult acetabular fracture
- Can help calculate Waldenstrom’s sign as below, which is a non-specific indicator for joint effusion
- Abnormal if >11mm or >2mm difference from contralateral hip
- Can help calculate acetabular angle as below
Acetabular Angle
- Angle measured from Hilgenreiner’s line/teardrop sign to line intersecting most superolateral aspect of acetabular rooft as depicted above
- Measurement taken from Hilgenreiner’s line (prior to ossification) in children vs. inferior margin of teardrop sign (after ossification) in adults.
- Children: angle <28º at birth, >22º after 1 year
- Decreased angle: Down syndrome, achondroplasia
- Increased angle: developmental dysplasia of hip
- Adults: normal range is 33º to 38º
- Increased angle: neuromuscular disorders
Joints
1. Sacroiliac: 2-4mm, equal bilaterally
2. Pubis symphysis < 5mm
3. Hip (femoral/acetabular): 3-5mm
- Suspicion for dislocation based on image results:
- If femoral head is superolateral to joint space and appears smaller than contralateral femoral head, it indicates a posterior dislocation; the majority of dislocations are posterior dislocations and they can lead to sciatic nerve damage.
- If femoral head is inferomedial to joint space and appears larger than contralateral femoral head, it indicates an anterior dislocation; anterior dislocations can damage the femoral nerve and artery.
Soft Tissues
- Periosteal swelling
- Fat pads
- Gluteus minimus fat stripe - superior aspect of femoral neck
- Bulging of this pad may indicate presence of effusion in hip joint
- Iliopsoas - inferior to iliopsoas tendon
- Bulging of this pad may indicate presence of effusion in hip joint
- Obturator fat strip - iliopectineal line
- Displacement or bulging may indicate pelvic sidewall hematoma secondary to a fracture
Common Fracture Patterns
Because the pelvis is a ring-like structure, be wary that a fracture in one part of the ring is often accompanied by damage to bone, ligament or tendon structures at some other point in the structure.
Usually low-energy fractures have only one break in the ring, and there is usually maintained alignment of the broken ends. In this case, there is low likelihood of the bones dislocating abruptly and causing damage to underlying structures, in which case these are considered stable pelvic fractures. These fractures can usually be managed non-operatively.
In the instance of high-speed motor vehicle collisions or other high-energy mechanisms, be concerned about pelvic injuries that involve two or more breaks in the pelvic ring. Often, if broken in multiple places in the structure, these fractures will be displaced and unstable, causing increased risk of damage to underlying structures. Patterns that have been identified to be unstable are noted in the classification system below
+ Bonus Tips - Avulsion Fractures
Fragment of bone is pulled away at the ligamentous or tendinous attachment due to damage of ligament or tendon, respectively
- Iliac crest - external abdominal oblique
- Anterior superior iliac spine - sartorius
- Anterior inferior iliac spine - rectus femoris
- Ischial tuberosity - hamstrings
- Inferior pubic ramus - adductors
- Greater trochanter of femur - gluteus medius and minimus
- Lesser trochanter - iliopsoas
Fracture Classifications (Young Burgess System)
A/P Compression (Head on mechanism)
APC I
Symphysis widening <2.5cm
- No posterior instability
- Non-operative management
- Weight bearing as tolerated
APC II/III
- Symphysis widening >2.5cm
- +/- Posterior stability
- *posterior instability = open book fracture
- require pelvic binders to prevent hemorrhage into increased pelvic space
- operative management
Lateral Compression (Side on mechanism)
LC I
SI joint compression without ligament rupture
- Non-operative management
- Weight bearing as tolerated
LCII/III
- SI joint rupture +/- APC injury to contralateral hemipelvis
- Operative management
- Pelvic binders can theoretically worsen this injury, however it concern for unstable fracture and unable to confirm, better to stabilize with a binder and confirm with plain imaging when able
Vertical Shear Fractures (axial load mechanism)
VS
- Displaced fractures of the anterior rami and posterior columns, including SI dislocation
- Operative management
- Traction often required acutely to stabilize hemipelvis location
Pediatric Quick Hits
+ Developmental Dysplasia of the Hip
A disorder of abnormal development resulting in dysplasia and possible subluxation or dislocation of the hip secondary to capsular laxity and mechanical factors
- Age group: most common <3mos, data-preserve-html-node="true" but can have late presentation in walking children as well
- Gender prevalence: 8F:1M
- Clinical history: positive ortolani, barlow test. Limitations in hip abduction due to laxity, and then in later presentation, stiffness
- Diagnosis: AP plain radiograph is primary imaging modality at 4-6 months after the femoral head begins to ossify. Use ultrasound prior to this age. Femoral head should be inferior ot Hilgenreiner's line and medial to Perkin's line with continuous Shenton's line
- Treatment: Pavlik harness for <6mos data-preserve-html-node="true" and reducible hip, closed reduction and spica casting for 6-18mos of age, open reduction and spica casting >18mos
+ Legg-Calvé-Perthes
Idiopathic avascular necrosis occurs secondary to disruption of blood supply to femoral head
- Age group: 5-6yo most common
- Gender prevalence: 5M:1F
- Clinical history: insidious onset in atraumatic hip, and patient presents with thigh or knee pain, or limp. Pain worsens with activity and is relieved by rest.
- Diagnosis: AP and frog leg views: medial joint space widening (measuring between teardrop and ossification center), irregular femoral head ossification
- Treatment: The younger the patient, the better the diagnosis. There are non-operative versus operative nuances, but in general, younger patients are non-operative with conservative management such as non-weight bearing and prescription of NSAIDs with referral to physical therapy.
+ Slipped Capital Femoris Epiphysis
A disorder of the growth plate that leads to slippage of the proximal portion of the femur, leading to anatomical dispositioning of the femoral head
- Age group: girls (8-15yo), boys (10-17yo); obese adolescents around the time of puberty
- Gender prevalence: 2M:1.4F
- Clinical history: patient presents with hip, knee or groin pain progressing to limp. Can progress over several weeks to months. Patient may present with external rotation of hip, unable to bear weight and limited range of motion
- Diagnosis: AP and frog leg; Klein's line will intersect less of the femoral head or not at all
- Treatment: surgical pinning
COntent and illustrations by Sim Mand, MD
Peer Editing and post by Ryan LaFollette, MD
References
- Bassett, A. “Slipped Capital Femoral Epiphysis.” Orthobullets. https://www.orthobullets.com/pediatrics/4040/slipped-capital-femoral-epiphysis?expandLeftMenu=true
- Campbell, SE. “Radiography of the hip: lines, signs and patterns of disease.” Seminars in Roentgenology. 2005 Jul; 40(3): 290–319.
- “Chapter 6: Basic Approach to Hip/Pelvis X-Ray.” Emergency Medicine Images for Practice: An Overview of X-Ray, Ultrasound, CT, and MRI Images, by Mari Baker.
- Chiamil, Sara Muñoz, and Claudia Astudillo Abarca. “Imaging of the Hip: A Systematic Approach to the Young Adult Hip.” Muscles, Ligaments and Tendons Journal 6.3 (2016): 265–280. PMC.
- Clohisy JC, Carlisle JC, Beaulé PE, et al. A Systematic Approach to the Plain Radiographic Evaluation of the Young Adult Hip. The Journal of Bone and Joint Surgery American volume. 2008;90(Suppl 4):47-66. doi:10.2106/JBJS.H.00756.
- Khurana B, Sheehan SE, Sodickson AD, Weaver MJ. “Pelvic Ring Fractures: What the Orthopedic Surgeon Wants to Know.” RSNARadiographics. 2014 Oct.
- Lim, Seung-Jae, and Yoon-Soo Park. “Plain Radiography of the Hip: A Review of Radiographic Techniques and Image Features.” Hip & Pelvis 27.3 (2015): 125–134. PMC.
- “Pelvic Fractures.” OrthoInfo: Diseases&Conditions; American Academy of Orthopedic Surgeons. https://orthoinfo.aaos.org/en/diseases--conditions/pelvic-fractures/
- “Radiology of the hip.” Wheeless Textbook of Orthopaedics Online, www.wheelessonline.com/ortho/radiology_of_the_hip
- Souder, C. “Developmental Dysplasia of the Hip.” Orthobullets. https://www.orthobullets.com/pediatrics/4118/developmental-dysplasia-of-the-hip?expandLeftMenu=true
- Souder, C. “Legg-Calve-Perthes Disease (Coxa plana).” Orthobullets. https://www.orthobullets.com/pediatrics/4119/legg-calve-perthes-disease-coxa-plana
- Weatherford, B. “Pelvic Ring Fractures.” Orthobullets. http://www.orthobullets.com/trauma/1030/pelvic-ring-fractures