Serotonin Syndrome & NMS
/Serotonin Syndrome
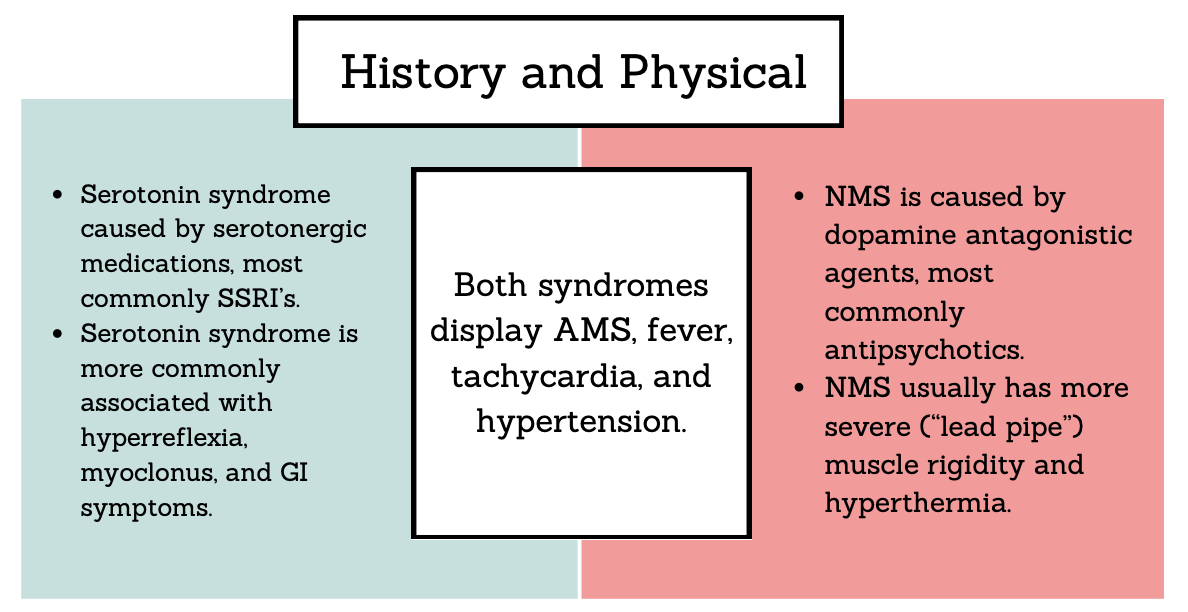
Serotonin Syndrome is also known as serotonin toxicity caused by increased serotonergic activity leading to a classic triad of AMS, autonomic hyperactivity, and neuromuscular abnormalities
Causative agents (all lead to stimulation of 5-HT receptors)
Antidepressants (SSRIs, SNRIs and MAOIs) - most common
Analgesics (fentanyl, methadone, and tramadol)
Antiemetics (ondansetron and metoclopramide)
Cold medications (dextromethorphan and pseudoephedrine)
Illicit substances (cocaine, ecstasy, methamphetamine, LSD)
Others (triptans, ergots, bromocriptine, linezolid, carbamazepine, cyclobenzaprine and methylene blue)
History to Gather
Detailed medication history including new medications, change in dosing, illicit substance use, and supplementation.
Timing of ingestion - syndrome presents within 6-24 hours of intake
Physical Exam Findings
Vital sign abnormalities: tachycardia, hypertension, hyperthermia
General: confused or agitated, tremulous
HEENT: ocular clonus, mydriasis
Skin: diaphoresis
GI: vomiting and diarrhea
Neuro: hyperreflexia and muscle clonus
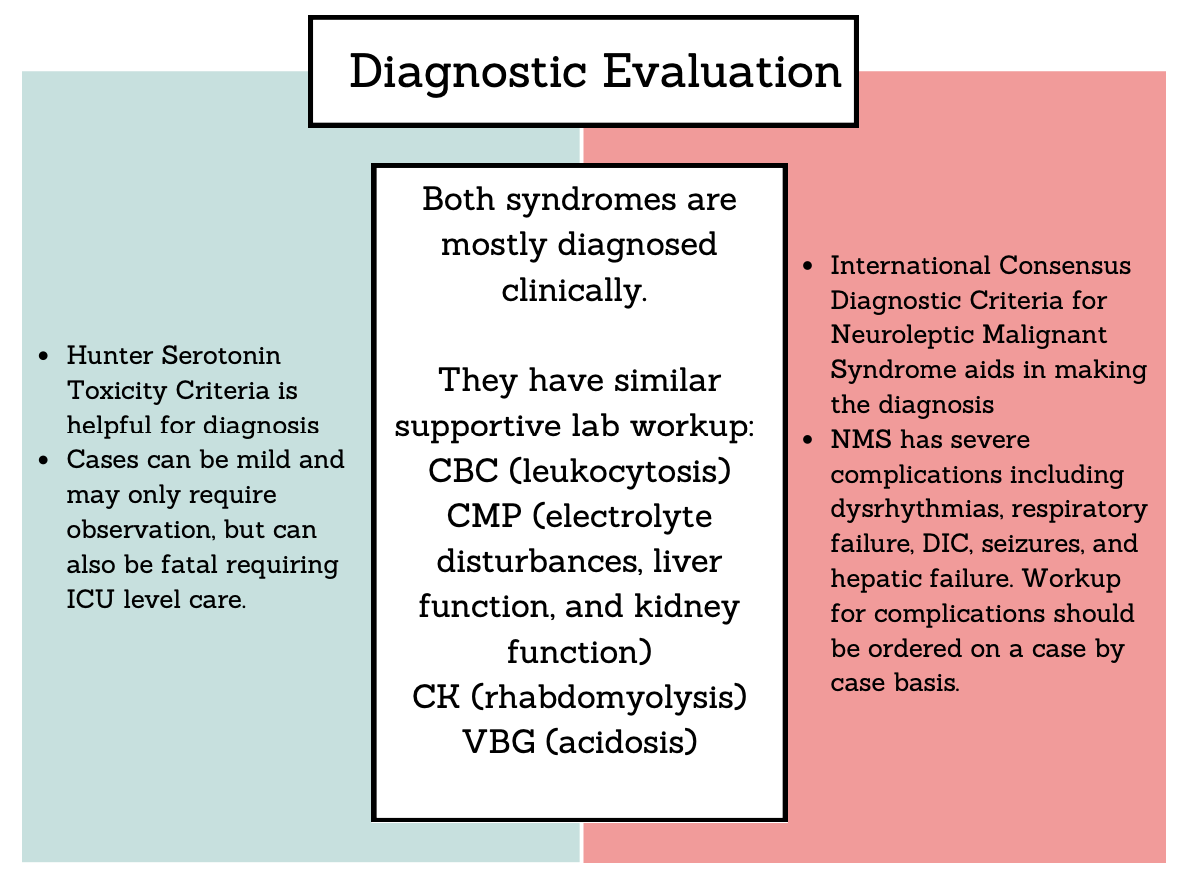
Evaluation
Clinical diagnosis using Hunter Serotonin Toxicity Criteria
Lab workup:
CBC - commonly have leukocytosis
BMP - assess for electrolyte abnormalities and renal dysfunction
CK - assess for rhabdomyolysis
VBG (in more severe cases) - may develop acidosis
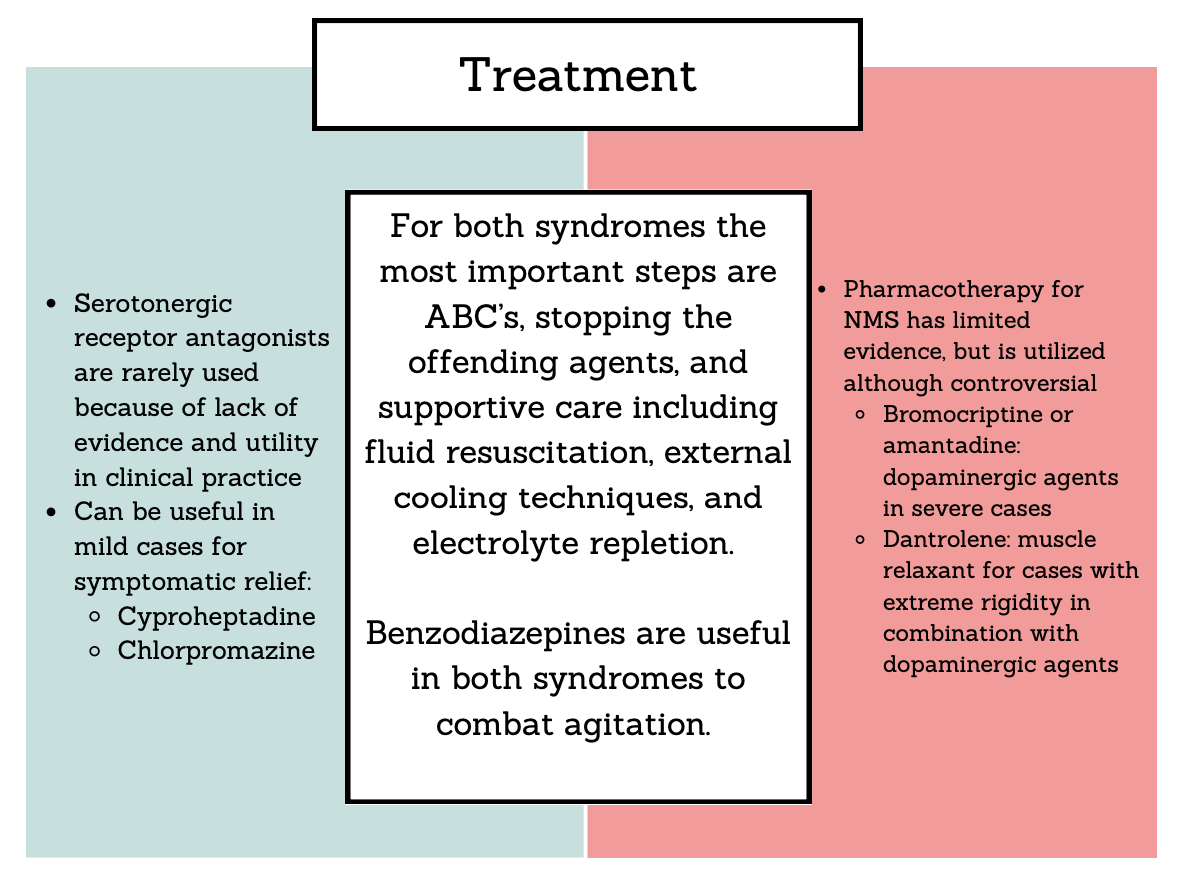
Management
Mainstay treatment: discontinue causative agent supportive care
IVF if dehydrated
External cooling measures, as antipyretics are ineffective
O2 as needed
Benzodiazepines for agitation (Dexmedetomidine for more severe cases, limited evidence
Other considerations:
For severe/refractory autonomic instability - esmolol, nicardipine or nitroprusside for extreme hypertension refractory to pain/agitation control
Pressors for hypotension (avoid dopamine)
Serotonergic receptor antagonists - rarely used clinically
Cyproheptadine - no controlled studies and limited evidence, only available orally
Has been showed to improve symptoms in mild cases
12 mg initially followed by 2mg q2hr
Chlorpromazine - very limited evidence, can be given IM
Risk of hypotension and dystonic reactions
Do not give if NMS is on differential
Disposition
Cases can range from mild, only requiring observation, to severe, requiring ICU level care. Generally, patients recover fully. The duration of symptoms depends on the causative agent and its pharmacology. Patients can be safely discharged when vital signs have normalized and patient has returned to mental status baseline with no signs of hyperreflexia or clonus.
Hunter Serotonin Toxicity Criteria (Sensitivity: 84% Specificity: 97%)
Must have recent exposure to a serotonergic drug plus 1 of the following:
Spontaneous clonus
Inducible clonus AND (agitation or
diaphoresis)
Ocular Clonus AND (agitation or
diaphoresis)
Tremor AND hyperreflexia
Hypertonia AND temperature >38 AND
(ocular clonus or inducible clonus)
Neuroleptic Malignant Syndrome
Neuroleptic Malignant Syndrome - caused by dopamine antagonism or rapid withdrawal of dopamine agonist medications, leading to AMS, muscle rigidity, fever, and autonomic instability. Between 0.01-0.04% of all patients treated with antipsychotics develop NMS
Causative agents
Intoxication with the following:
All antipsychotics
Antiemetics (Droperidol,
Domperidone, Metoclopramide,
Promethazine, Prochlorperazine)
Others (Tetrabenazine, Reserpine, Amoxapine, Diatrizoate, Lithium,
Phenelzine, Dosulepin, Trimipramine, Desipramine)
Rapid withdrawal from the following:
Levodopa
Amantadine
Tolcapone
History - Detailed medication history including new medications, change in dosing, illicit substance use, and supplementation.
Physical Exam
Vital sign abnormalities: tachycardia, hypertension, hyperthermia
General: confused or agitated, tremulous
Skin: diaphoresis
Neuro: “lead pipe” rigidity, dystonia, dysphagia, dysarthria
Evaluation
Clinical diagnosis - International Consensus Diagnostic Criteria for Neuroleptic Malignant Syndrome is helpful
Lab workup
CBC - commonly have leukocytosis
CMP - assess for electrolyte abnormalities, liver dysfunction, and renal dysfunction
CK - assess for rhabdomyolysis
VBG (in more severe cases) - may develop acidosis
Management
Discontinue causative agent if dopamine antagonist toxicity or restart dopaminergic agent if rapid withdrawal is the cause of NMS
Supportive care
IVF if dehydrated
External cooling measures, as antipyretics are ineffective
O2 as needed
Benzodiazepines for agitation
Specific pharmacotherapy (controversial):
Bromocriptine or amantadine: dopaminergic agents, some meta-analysis and case reports show decreased mortality in severe cases
Bromocriptine: 2.5mg PO q8-12hr, max dose 45mg/day
Amantadine: 100mg PO initially; max dose 200mg q12hr
Dantrolene: muscle relaxant for cases with extreme rigidity, use in combination (not as monotherapy) with dopaminergic agents in severe cases
1-2.5 mg/kg initially followed by 1mg/kg q6hrs
Disposition
NMS can be very severe and usually requires ICU level care.
Potential complications include dysrhythmias, respiratory failure, DIC, seizures, and hepatic failure. Workup for complications should be initiated on a case by case basis.
International Consensus Diagnostic Criteria for Neuroleptic Malignant Syndrome > 74 points (out of 100) used to determine presence of NMS (Sensitivity: 69.6% Specificity: 90.7%)
Exposure to a dopamine antagonist or withdrawal of a dopamine agonist in the prior 72 hours: 20 points
Hyperthermia (>100.4 F or >38C) on at least two occasions, measured orally: 18 points
Rigidity: 17 points
Mental status alteration (reduced or fluctuating level of consciousness): 13 points
Creatinine kinase elevation at least four times the upper limit of normal: 10 points
Sympathetic nervous system lability, defined as at least two of the below: 10 points
Blood pressure elevation (systolic or diastolic >25% above baseline)
Blood pressure fluctuation (>25% systolic or >20% diastolic change in 24 hours)
Diaphoresis
Urinary incontinence
Hypermetabolic state (defined as heart rate increase >25% above baseline and respiratory rate increase >50% above baseline): 5 points
Negative evaluation for other toxic, metabolic, infectious, or neurologic causes: 7 points
Differentiating Serotonin Syndrome and NMS
References
Chiew AL, Isbister GK. Management of serotonin syndrome (toxicity). Br J Clin Pharmacol. 2024; 1-8. doi:10.1111/bcp.16152
Dunkley EJ, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The Hunter serotonin toxicity criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM 2003; 96:635–642.
Gillman PK. Successful treatment of serotonin syndrome with chlorpromazine. Med J Aust 1996; 165:345–346.
Gurrera RJ, Mortillaro G, Velamoor V, Caroff SN. A Validation Study of the International Consensus Diagnostic Criteria for Neuroleptic Malignant Syndrome. J Clin Psychopharmacol. 2017 Feb;37(1):67-71. doi: 10.1097/JCP.0000000000000640. PMID: 28027111.
Iqbal MM, Basil MJ, Kaplan J, Iqbal MT. Overview of serotonin syndrome. Ann Clin Psychiatry 2012; 24:310–318.
Kornhuber J, Weller M: Neuroleptic malignant syndrome. Curr Opin Neurol 1994, 7:353-357.
Kuhlwilm L, Schönfeldt-Lecuona C, Gahr M, Connemann BJ, Keller F, Sartorius A. The neuroleptic malignant syndrome-a systematic case series analysis focusing on therapy regimes and outcome. Acta Psychiatr Scand. 2020 Sep;142(3):233-241. doi: 10.1111/acps.13215. Epub 2020 Aug 2. PMID: 32659853.
Nguyen H, Pan A, Smollin C, Cantrell LF, Kearney T. An 11-year retrospective review of cyproheptadine use in serotonin syndrome cases reported to the California Poison Control System. J Clin Pharm Ther. 2019; 44(2): 327-334. doi:10.1111/jcpt.12796
Reulbach, U., Dütsch, C., Biermann, T. et al. Managing an effective treatment for neuroleptic malignant syndrome. Crit Care 11, R4 (2007). https://doi.org/10.1186/cc5148
Strawn, J. R., Keck, P. E., & Caroff, S. N. (2007). Neuroleptic Malignant Syndrome. American Journal of Psychiatry, 164(6), 870–876. https://doi.org/10.1176/ajp.2007.164.6.870
Simon LV, Torrico TJ, Keenaghan M. Serotonin Syndrome. [Updated 2024 Mar 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482377/
Simon LV, Hashmi MF, Callahan AL. Neuroleptic Malignant Syndrome. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482282/
Authorship
Written by, Graphics by: Victoria Martell, MD PGY-1, University of Cincinnati Department of Emergency Medicine
Peer Review, Editing, Posting by: Jeffery Hill, MD MEd, Associate Professor, University of Cincinnati Department of Emergency Medicine
Cite as: Martell, V., Hill, J., Serotonin Syndrome & NMS. TamingtheSRU. www. tamingthesru.com/blog/core-content/serotonin-syndrome-amp-nms. 1/5/2025.






