Prehospital TBI - Beyond the "Code"
/Of the injuries that one will care for in the pre-hospital setting, traumatic brain injury is one of the most challenging. Quite often, more than one organ system has been injured and they require rapid, thoughtful, and precise management of their airway and hemodynamics. In addition, TBI patients require frequent reassessment to detect progression of the primary neurologic injury. This is easier said than done in the dynamic, unpredictable, and resource-limited prehospital environment.
To help simplify their care, the following “Code of Care” forms the core principles that characterize optimal TBI care:
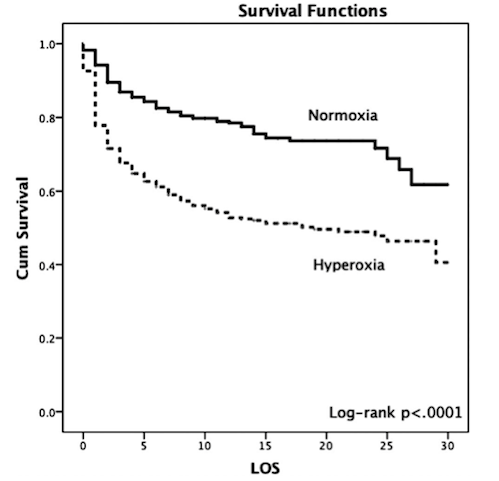
- NO Hypoxia (SpO2 < 90%) – therefore, apneic oxygenation for all TBI patients
- NO Hypotension (sBP < 90 mmHg) – greatest iatrogenic risk is with induction and provision of positive pressure ventilation
- Blown pupil -> Hyperosmotic therapy + Hyperventilate